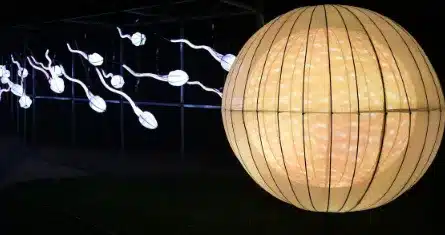
Fertility surgery encompasses procedures like ovarian drilling, sperm retrieval, and egg retrieval, aimed at addressing infertility issues. Ovarian drilling involves making small holes in the ovarian surface to stimulate ovulation in women with polycystic ovary syndrome (PCOS), while sperm retrieval and egg retrieval are vital steps in assisted reproductive technologies (ART) such as in vitro fertilization (IVF), assisting couples struggling with conception.
What is Fertility Surgery?
Fertility surgery, also known as reproductive surgery, refers to surgical interventions performed to treat infertility or improve the chances of conception. These procedures aim to correct anatomical abnormalities, remove obstructions, or address underlying medical conditions that hinder fertility. Fertility surgery can be performed on both women and men, targeting specific reproductive organs and structures to optimize their functionality and increase the likelihood of successful conception.
Clinic contact number: +989371200167
Female Fertility Surgeries
- Hysteroscopy: This minimally invasive procedure involves inserting a thin, lighted tube (hysteroscope) through the vagina and cervix to examine and treat conditions affecting the uterus, such as uterine polyps, fibroids, adhesions, or septum.
- Laparoscopy: Laparoscopic surgery is performed by making small incisions in the abdomen and inserting a thin camera (laparoscope) to visualize and treat conditions like endometriosis, ovarian cysts, adhesions, or blocked fallopian tubes.
- Tubal surgeries: Fallopian tube surgeries aim to repair or remove blockages, correct tubal deformities, or perform tubal ligation reversal (reversing a previous sterilization procedure) to restore fertility.
- Ovarian surgeries: Procedures like ovarian drilling, ovarian cystectomy (removal of cysts), or ovarian wedge resection are performed to treat polycystic ovary syndrome (PCOS) or remove ovarian tumors, thereby improving ovarian function.
- Myomectomy: Myomectomy involves the removal of uterine fibroids while preserving the uterus, allowing women with fibroids to retain their fertility.
Surgical Infertility Treatment Overview
Fertility surgeries can address various underlying conditions contributing to infertility in women and men. These surgeries are often recommended after less invasive unsuccessful treatments or when a specific anatomical issue is identified.
Before opting for surgery, thorough diagnostic evaluations and discussions with fertility specialists are crucial to determine the most appropriate action.
Female Infertility Conditions Treated by Surgery
Female infertility conditions treated by surgery include endometriosis, uterine fibroids, uterine septum, ovarian cysts, blocked fallopian tubes, and pelvic adhesions.
Fallopian tube obstruction
Surgery can repair tubal blockages caused by pelvic inflammatory disease, endometriosis, or previous pelvic surgeries.
Uterine abnormalities
Surgical interventions correct uterine septum (a wall dividing the uterus), uterine fibroids, polyps, or structural anomalies that affect implantation or pregnancy maintenance.
Endometriosis
Laparoscopic surgery can remove endometrial tissue implants and adhesions, restoring fertility in women affected by this condition.
Polycystic ovary syndrome (PCOS)
Ovarian drilling is a minimally invasive procedure that treats PCOS by puncturing the ovaries to reduce androgen production and restore ovulation.
Ovarian cysts or tumors
Surgical removal of cysts or tumors can restore ovarian function and improve fertility prospects.

Male Fertility Surgeries
Male fertility surgeries include varicocele repair, vasectomy reversal, testicular sperm extraction (TESE), and surgical correction of obstructive reproductive tract anomalies.
Varicocele repair
Varicoceles are enlarged veins in the scrotum that can impair sperm production. Surgery aims to ligate or redirect blood flow, improving sperm quality and count.
Vasectomy reversal
Men who have previously undergone vasectomy can opt for surgical procedures to reconnect the vas deferens, enabling the passage of sperm and restoring fertility.
Ejaculatory duct obstruction repair
Obstruction in the ejaculatory ducts, which transport sperm from the testicles, can be treated surgically to allow the passage of sperm during ejaculation.
Testicular sperm extraction (TESE)
In cases where sperm is absent in the ejaculate due to testicular dysfunction, TESE involves extracting sperm directly from the testes for use in assisted reproductive techniques.
Treatments
Apart from surgery, various assisted reproductive technologies (ART) can be used with fertility surgery to enhance the chances of conception. These treatments include:
- Intrauterine Insemination (IUI): Sperm is processed and placed directly into the uterus during the woman’s fertile period.
- In Vitro Fertilization (IVF): Eggs are retrieved from the woman’s ovaries, fertilized with sperm in a laboratory, and the resulting embryos are transferred to the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected directly into an egg to facilitate fertilization in severe male factor infertility cases.
- Gamete Intrafallopian Transfer (GIFT): Eggs are mixed with sperm and inserted into the fallopian tubes, allowing fertilization to occur naturally within the woman’s body.
Fertility surgery may be recommended when other non-surgical fertility treatments (such as medications or assisted reproductive techniques) are not effective or suitable for the underlying cause of infertility.
Some types of tubal surgery may be performed through the laparoscope, while other procedures (such as tubal surgery) may require microsurgery. IVF Australia
10 Risks of Fertility Treatment for Women
- Multiple pregnancies: Using fertility surgery medications and ART increases the risk of conceiving twins, triplets, or higher-order pregnancies, leading to complications for both the mother and babies.
- Ovarian hyperstimulation syndrome (OHSS): Intensive ovarian stimulation during fertility treatments can result in swollen, painful ovaries and fluid accumulation in the abdomen and chest.
- Ectopic pregnancy: Fertility surgery slightly increase the risk of ectopic pregnancies, where the fertilized egg implants outside the uterus, typically in the fallopian tubes.
- Miscarriage: The risk of miscarriage remains elevated in women undergoing fertility treatments compared to those conceiving naturally.
- Adverse reactions to medications: Fertility medications can cause side effects such as mood swings, hot flashes, bloating, or allergic reactions.
- Pelvic infection: In rare cases, fertility procedures can introduce bacteria into the reproductive system, leading to infections.
- Ovarian torsion: Ovarian stimulation and enlarged ovaries increase the risk of ovarian twisting (torsion), which requires immediate medical attention.
- Damage to surrounding organs: Surgical fertility procedures, although rare, can carry risks of damaging nearby organs such as the bladder, bowel, or blood vessels.
- Emotional and psychological stress: The emotional toll of fertility treatments can be significant, leading to stress, anxiety, and depression.
- Financial burden: Fertility treatments, including surgery and ART, can be expensive and may not be covered by insurance, placing a financial strain on couples seeking assistance.
Clinic contact number: +989371200167
10 Risks of Fertility Treatments for Men
- Infection: Fertility procedures carry a small risk of infection in the reproductive organs, although the incidence is relatively low.
- Discomfort and pain: Following surgery or specific procedures, men may experience temporary pain, swelling, or discomfort in the scrotum or testicles.
- Hematoma: Rarely bleeding or blood collection (hematoma) may occur at the surgical site or due to other interventions.
- Damage to surrounding structures: Surgical procedures, such as varicocele repair or vasectomy reversal, carry a slight risk of injury to adjacent blood vessels, nerves, or organs.
- Recurrence or persistence of fertility issues: In some cases, despite surgery or treatment, fertility problems may persist or recur, necessitating further interventions.
- Adverse effects of medications: Fertility medications used in men can lead to side effects like mood changes, acne, or changes in sexual function.
- Psychological impact: Men undergoing fertility treatments may experience emotional stress, anxiety, or depression due to the challenges of infertility and treatment.
- Semen quality changes: Some fertility treatments can temporarily affect sperm parameters, resulting in changes in sperm count, motility, or morphology.
- Genetic concerns: In cases where genetic testing or screening is recommended, there is a possibility of identifying genetic abnormalities that may have implications for future offspring.
- Financial considerations: Like women, men may face financial burdens associated with fertility treatments, including surgeries, medications, and assisted reproductive techniques.
The Role of Minimally Invasive Techniques in Modern Fertility Surgery
Fertility surgery is a critical component of reproductive medicine, focusing on procedures that address obstructions and abnormalities in the reproductive system to enhance fertility. Esteemed institutions like Stanford University and Harvard Medical School are at the forefront of research and education in this specialized field. Prominent figures such as Dr. Robert Edwards, a pioneer in reproductive medicine, have significantly contributed to the development and success of surgical interventions aimed at improving fertility outcomes.
In terms of active healthcare providers, the Center for Reproductive Medicine and Fertility in New York is recognized for its high volume of fertility surgeries and exceptional success rates. Recent statistics from this center indicate a significant improvement in pregnancy outcomes following hysteroscopic and laparoscopic surgeries, which are commonly employed to treat conditions like endometrial polyps, uterine septa, and tubal blockages. With advancements in minimally invasive surgical techniques, the field has seen a notable decrease in patient recovery time and an increase in the overall efficacy of fertility-enhancing procedures.
Summary
In conclusion, fertility surgery offers hope to couples facing challenges in conceiving naturally, employing a range of techniques such as ovarian drilling, sperm retrieval, and tubal ligation reversal. Ovarian drilling, often performed laparoscopically, proves effective in managing conditions like polycystic ovary syndrome (PCOS) by inducing ovulation.
Similarly, procedures like sperm retrieval and tubal ligation reversal, often carried out through laparoscopy or hysteroscopy, facilitate conception by addressing specific barriers to fertility. These interventions not only enhance the chances of successful pregnancy but also provide couples with renewed optimism on their journey towards parenthood.

Fun fact: Did you know that the fascinating world of fertility surgery extends beyond just surgeries? While procedures like Tubal Ligation Reversal, Endometriosis Surgery, and Varicocele Repair directly restore reproductive health, there are alternative paths too!
Some couples might explore options like In Vitro Fertilization (IVF), where the magic happens outside the body. Others might rely on the subtle nudge from Ovulation Inducing Medications such as Clomid to boost their chances. And guess who’s orchestrating this intricate dance of treatments?
The Reproductive Endocrinologist! They’re the maestros of this realm, guiding hopeful couples through surgical and non-surgical avenues to parenthood. The journey to bringing life is as diverse as life itself!
Clinic contact number: +989371200167
FAQs
1. Is fertility surgery the only option for treating infertility? No, fertility surgery is not the only option. Depending on the cause of infertility, other treatments like fertility medications, lifestyle changes, or assisted reproductive technologies (ART) may also be recommended.
2. Are the risks associated with fertility treatments significant? While the risks exist, it’s important to note that most individuals undergoing fertility treatments do not experience severe complications.
3. What are the common types of fertility surgery for men? Common fertility surgeries for men include:
- Varicocele repair to treat enlarged veins in the scrotum that can affect sperm production.
- Vasectomy reversal to restore fertility after a previous vasectomy.
- Surgical retrieval of sperm from the testes (testicular sperm extraction or TESE) for use in assisted reproductive techniques.
4. When is fertility surgery recommended? Fertility surgery may be recommended when other non-surgical fertility treatments (such as medications or assisted reproductive techniques) are not effective or suitable for the underlying cause of infertility. It is often used to correct structural abnormalities that impair fertility.
5. How is fertility surgery performed? Fertility surgery can be performed using minimally invasive techniques (such as laparoscopy or hysteroscopy) or traditional open surgery, depending on the specific condition and complexity of the procedure. The goal is to correct anatomical issues while minimizing trauma and recovery time.
Fertility surgery | IVF Australia




