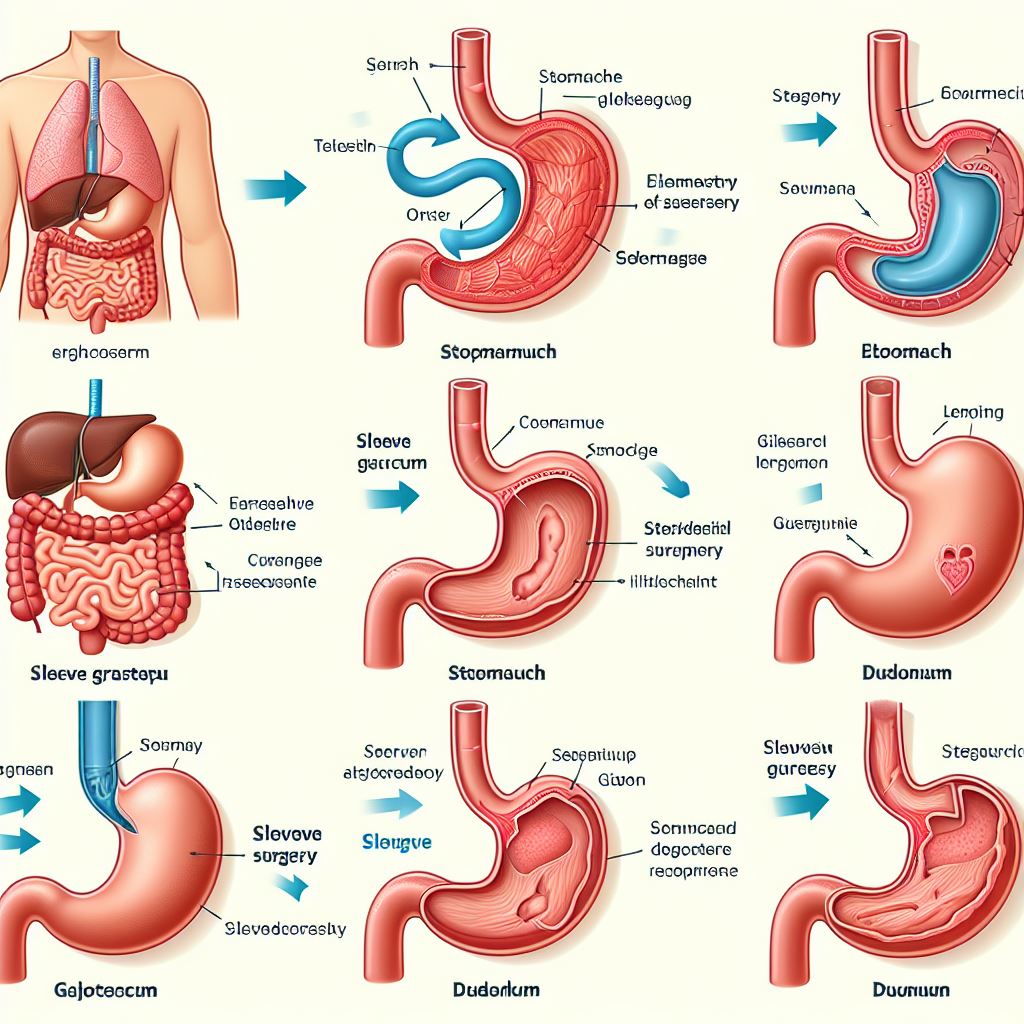
Gastric sleeve surgery, like any other surgical procedure, carries certain risks and potential complications. Preoperative risks involve understanding and managing complications that may arise before the surgery itself. These can include blood clots, infections, or adverse reactions to anesthesia. It is crucial for both patients and healthcare professionals to be aware of these risks in order to mitigate them effectively.
During the surgical procedure, there are risks of surgical complications that may occur. These can range from bleeding and organ injury to infection. Just like any invasive procedure, these risks are generally low, but they should still be taken into consideration. Surgeons and their teams work diligently to minimize these risks by following strict protocols and ensuring the utmost care and precision during the surgery. By being aware of these potential complications, patients can make informed decisions about their treatment options.
Preoperative Risks: Understanding the potential complications that may arise before the surgery, such as blood clots, infections, or adverse reactions to anesthesia.
Preoperative Risks: Understanding the potential complications that may arise before the surgery, such as blood clots, infections, or adverse reactions to anesthesia.
Before undergoing gastric sleeve surgery, it is crucial to be aware of the potential risks and complications that may occur during the preoperative phase. One significant concern is the formation of blood clots, also known as deep vein thrombosis (DVT). This risk is particularly elevated for individuals with a history of blood clotting disorders, obesity, or a sedentary lifestyle. Therefore, it is important for patients to receive appropriate guidance and preventive measures, such as early mobilization and blood-thinning medications, to minimize the possibility of DVT.
Additionally, infections pose another potential risk during the preoperative period. Surgical site infections can occur if proper hygiene practices are not followed or if a preexisting infection is present and not properly treated. To mitigate this risk, patients may receive thorough preoperative assessments to identify any underlying infections and receive appropriate treatment beforehand. Furthermore, adherence to rigorous sterile protocol during surgery can significantly reduce the likelihood of developing infections. Finally, adverse reactions to anesthesia, although rare, are also a potential concern. Prior to surgery, patients should inform their healthcare providers about any known allergies or previous adverse reactions to anesthesia to ensure a safe and tailored administration during the procedure.
Surgical Complications: Exploring the possible risks during the surgical procedure, including bleeding, organ injury, or infection.
During gastric sleeve surgery, there are several potential risks and complications that can occur. One of the most common risks is bleeding, which can be caused by the incisions made during the procedure. While the surgical team takes precautions to minimize bleeding, it can still occur and may require additional measures to control it. Another possible complication is organ injury, which can happen when the surgeon is manipulating the stomach or other nearby organs. Although rare, it is a risk that must be considered before undergoing the surgery. Additionally, infection is always a concern with any surgical procedure. The surgical site can become infected, leading to complications and prolonged recovery. To mitigate this risk, surgeons and healthcare professionals follow strict protocols to maintain a sterile environment during the surgery.
In conclusion, while gastric sleeve surgery is generally considered safe, there are potential risks and complications that patients should be aware of. Bleeding, organ injury, and infection are some of the possible risks during the surgical procedure. It is essential for individuals considering this procedure to have a comprehensive understanding of the potential complications and discuss them with their healthcare team. By being well-informed, patients can make informed decisions and take necessary steps to minimize risks during their gastric sleeve journey.
Postoperative Infections: Discussing the likelihood of developing infections after the surgery and the measures taken to prevent and treat them.
Postoperative infections are a potential concern following gastric sleeve surgery. Due to the nature of the procedure, there is a risk of bacteria entering the body and causing infections. The surgical incisions made during the surgery can also provide an entry point for infection. Additionally, if proper hygiene and care measures are not followed after the surgery, the risk of infection can increase.
To mitigate the risk of postoperative infections, surgeons and medical staff take several measures. Prior to the surgery, patients are often prescribed antibiotics to reduce the chance of infection. During the operation, strict adherence to sterile techniques and using sterile instruments helps minimize the risk. After the surgery, patients are closely monitored for signs of infection, such as fever or increased pain. In case an infection does occur, it is promptly diagnosed and treated with appropriate antibiotics. Moreover, patients are educated about proper wound care and hygiene practices to minimize the risk of infection during the recovery period.
Nutritional Deficiencies: Highlighting the risk of nutrient deficiencies due to decreased food intake and absorption, and the importance of proper supplementation.
Gastric sleeve surgery, a popular weight loss procedure, comes with its fair share of potential risks and complications. One of the risks associated with this surgery is the development of nutritional deficiencies. Due to the decreased food intake and absorption capacity of the stomach after the surgery, patients may face challenges in obtaining the necessary nutrients to maintain good health.
When the size of the stomach is reduced, the amount of food a person can consume is significantly limited. As a result, there is a higher chance of not getting enough essential vitamins and minerals from dietary sources alone. Additionally, the altered anatomy of the gastrointestinal tract can affect the absorption of nutrients, further increasing the risk of deficiencies. In order to mitigate these risks, proper supplementation of essential nutrients under the guidance of a healthcare professional is crucial for patients who have undergone gastric sleeve surgery.
Dumping Syndrome: Explaining the occurrence of dumping syndrome, its symptoms, and how it can be managed.
Dumping syndrome is a common occurrence after gastric sleeve surgery. It happens when food, especially high-sugar or high-fat foods, moves too quickly from the stomach into the small intestine. This rapid emptying can cause a range of symptoms, including nausea, diarrhea, abdominal pain, dizziness, and sweating. Some individuals may also experience palpitations or rapid heartbeat. Although dumping syndrome can be uncomfortable and inconvenient, it can often be managed by making dietary changes. Consuming smaller, more frequent meals and avoiding foods that trigger symptoms, such as sweets, fatty foods, and alcohol, can help prevent or minimize the occurrence of dumping syndrome. In some cases, medication may be prescribed to manage symptoms or slow down the emptying of the stomach. It’s essential for individuals who have undergone gastric sleeve surgery to be aware of the possibility of dumping syndrome and work closely with their healthcare team to find effective management strategies.
Gastroesophageal Reflux Disease (GERD): Discussing the potential development or worsening of GERD after gastric sleeve surgery and the available treatment options.
Gastroesophageal Reflux Disease (GERD) is a condition characterized by the backward flow of stomach acid into the esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. While gastric sleeve surgery is an effective procedure for weight loss, it can potentially lead to the development or worsening of GERD in some patients. This occurs due to the changes made to the stomach during the surgery, which can affect the function of the lower esophageal sphincter, the muscle responsible for preventing acid reflux.
The potential development or aggravation of GERD after gastric sleeve surgery is a concern that needs to be carefully addressed by both patients and healthcare professionals. It is important for individuals considering the procedure to have a thorough understanding of this potential risk and the available treatment options. By being aware of the possibility of GERD, patients can work closely with their healthcare team to develop a personalized post-surgery plan that includes lifestyle modifications, dietary changes, and possibly medication to alleviate the symptoms and manage the condition effectively.
Stricture Formation: Addressing the possibility of the narrowing of the stomach outlet, causing difficulties in food passage and the need for corrective measures.
Stricture formation is one of the potential complications that may arise following gastric sleeve surgery. This condition occurs when the stomach outlet becomes narrowed, leading to difficulties in the passage of food. When a stricture develops, patients may experience symptoms such as nausea, vomiting, and a sensation of food getting stuck in the throat. Strictures can occur due to various factors, including the healing process after surgery, scar tissue formation, or inflammation. It is important to address this issue promptly to ensure the proper functioning of the stomach and prevent any further complications.
If a stricture is suspected, the healthcare provider may perform an evaluation, which may include an upper endoscopy or imaging tests. Treatment options for stricture formation vary depending on the severity of the condition. In some cases, the stricture may resolve on its own or with dietary modifications, such as consuming smaller meals. However, if the symptoms persist or worsen, further interventions may be necessary. These can involve the dilation of the strictured area using an endoscope or even surgical intervention to widen the narrowed passage. Close monitoring and follow-up care are essential to ensure that the stricture is successfully managed and that the patient can continue to eat and digest food normally.
Long-Term Weight Loss Maintenance: Exploring the challenges associated with sustaining weight loss after surgery and the strategies to overcome them.
Weight loss maintenance is a significant challenge for individuals who undergo gastric sleeve surgery. While the procedure provides an initial reduction in weight, sustaining this weight loss in the long term requires a dedicated approach. One of the main challenges is the potential for the stomach to stretch over time, allowing individuals to consume larger portions of food. To overcome this, healthcare professionals recommend a strict adherence to portion control and a focus on nutrient-dense, low-calorie foods. Additionally, incorporating regular physical activity into daily routines can help to prevent weight regain and support long-term weight management.
Another obstacle in long-term weight loss maintenance after gastric sleeve surgery is the psychological aspect. Many individuals may experience emotional and mental struggles following the procedure. These could include body image issues, anxiety, or fear of regaining weight. Seeking psychological support and counseling can significantly assist patients in navigating these challenges. Developing healthy coping mechanisms and addressing any underlying emotional concerns can facilitate sustainable weight loss and improve overall well-being.
Psychological Effects: Shedding light on the emotional and
Weight loss surgery can have significant psychological effects on individuals. While the physical changes are often the primary focus, the emotional impact should not be underestimated. Many patients experience a range of emotions before, during, and after gastric sleeve surgery.
For some, there may be feelings of excitement and anticipation as they embark on a journey towards a healthier lifestyle. However, it is not uncommon for individuals to also experience anxiety and fear as they ponder the uncertainties and potential challenges that lie ahead. The decision to undergo weight loss surgery is a deeply personal one, and it is essential for patients to have a support system in place to help navigate the emotional ups and downs that may arise throughout the process.
Post-surgery, patients may also grapple with a variety of emotional changes. It is not uncommon for individuals to experience a sense of loss, as their relationship with food undergoes a significant transformation. Food can often be a source of comfort or an emotional crutch, and the restrictions imposed by the surgery can lead to feelings of frustration or even sadness. Additionally, individuals may experience body image concerns or feelings of self-consciousness as they adjust to their new physical appearance. Emotional support and counseling can play a vital role in helping patients navigate these changes and develop a healthy mindset towards food and their body.
What are some potential complications that may arise before gastric sleeve surgery?
Some potential complications that may arise before gastric sleeve surgery include blood clots, infections, or adverse reactions to anesthesia.
What are the risks during the surgical procedure?
The risks during the surgical procedure may include bleeding, organ injury, or infection.
Is there a likelihood of developing infections after the surgery?
Yes, there is a likelihood of developing infections after the surgery. However, measures are taken to prevent and treat them.
How does gastric sleeve surgery affect nutrient intake and absorption?
Gastric sleeve surgery can lead to decreased food intake and absorption, which increases the risk of nutrient deficiencies. Proper supplementation is important in such cases.
What is dumping syndrome and how can it be managed?
Dumping syndrome is a condition that occurs after eating, causing symptoms like nausea and diarrhea. It can be managed by eating smaller, more frequent meals and avoiding certain foods.
Can gastric sleeve surgery lead to the development or worsening of GERD?
Yes, gastric sleeve surgery can potentially lead to the development or worsening of gastroesophageal reflux disease (GERD). There are available treatment options for managing GERD after surgery.
Is there a possibility of stricture formation after gastric sleeve surgery?
Yes, there is a possibility of the narrowing of the stomach outlet, known as stricture formation, which can cause difficulties in food passage. Corrective measures may be needed in such cases.
What are the challenges associated with sustaining weight loss after gastric sleeve surgery?
Sustaining weight loss after gastric sleeve surgery can be challenging due to factors such as lifestyle changes, emotional and psychological factors, and the need for long-term commitment to healthy habits.
How does gastric sleeve surgery impact a person’s emotional well-being?
Gastric sleeve surgery can have psychological effects on individuals, including changes in body image, self-esteem, and emotional well-being. These effects should be acknowledged and addressed for a successful recovery.